
Imagine a world where healthcare professionals spend more time with patients and less time buried under paperwork. Unfortunately, the reality often involves navigating around multiple administrative tasks that can drain time and resources. To reduce administrative burdens, healthcare providers should streamline their RCM.
In this blog, we'll explore the transformative power of revenue cycle management services in reducing administrative burdens. We will also uncover how these services streamline workflows, improve efficiency, and help healthcare professionals dedicate more time to delivering exceptional patient care.
What are the burdens of administrative tasks?
In the healthcare RCM world, it is vital to take prompt action at every step to avoid compliance or payment issues. According to Advocacy Consumer Reports, Americans reportedly spent $9,700 annually on healthcare, with approximately $720 attributed to administrative costs. Healthcare providers must follow all the regulations to avoid payment denials and penalties.
Picture this: stacks of paperwork awaiting processing, intricate billing codes to enter, and the endless back-and-forth of manual data entry. These are just a few snapshots of the administrative maze that healthcare providers navigate daily. Here are some of the other administrative burdens healthcare providers face.
Time-consuming paperwork
According to a report by the National Library of Medicine, healthcare providers spend 35% of their time on documentation and paperwork. From patient intake forms to insurance verification, paperwork is intense. Each form requires attention to detail, consuming valuable time that could be spent on patient care. Multiply this by the number of patients seen daily, and the administrative burden quickly becomes apparent.
Billing complexities
Medical billing and coding in healthcare are complex. It consists of many codes, modifiers, and regulations to navigate. From ensuring accurate coding to submitting claims within tight deadlines, there is no margin for errors. This leads to potential delays and revenue loss.
Manual processes
Despite advances in technology, many healthcare organizations still rely on manual processes for administrative tasks. This reliance on pen-and-paper methods or outdated systems slows down workflows and increases the risk of errors.
Impact on staff burnout
According to Beckers, 63% of healthcare providers face a shortage of skilled professionals. As the administrative burdens pile up, healthcare staff burnout the most. The constant juggling of patient care and paperwork can lead to burnout, affecting morale and productivity. When staff is burdened, errors become more likely, and healthcare workers might also quit their job.
Errors and financial inefficiencies
Inaccuracies in billing and documentation can have significant consequences, like denied claims and delayed payments. Healthcare providers get caught in a cycle of chasing down payments, solving discrepancies, and trying to streamline billing processes.
What is the role of RCM in reducing administrative burdens?
Optimizing revenue cycle management processes reduces administrative burdens and aids healthcare providers in surpassing their growth goals. It also streamlines the financial aspects of healthcare operations. Here is the essential role RCM plays for healthcare providers.
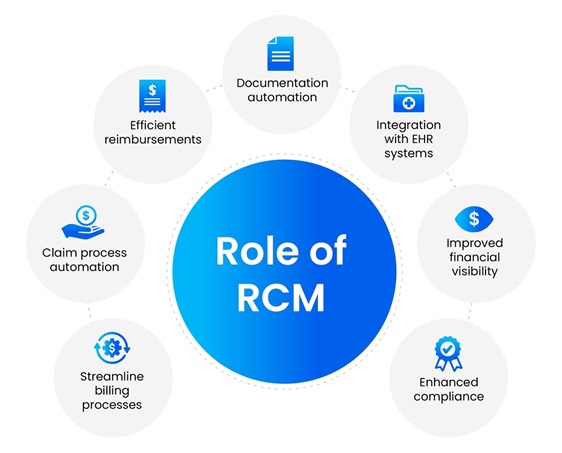
Streamline billing processes
At the heart of RCM lies the automation of billing processes. Say goodbye to tedious paper claims. With optimized RCM, billing becomes an efficient process.
Claim process automation
Submitting claims and tracking their progress becomes easy with technology. Automated workflows ensure that claims are submitted accurately and promptly, reducing denials and delays.
Efficient reimbursements
For healthcare providers, timely reimbursement is essential for financial stability. Revenue cycle management services streamline the reimbursement process, ensuring payments are received promptly.
Documentation automation
Gone are the days of drowning in a sea of paperwork. 65% of the hospitals in the US leverage AI in their revenue cycle management. Healthcare providers can automate documentation processes to reduce the need for manual data entry. It not only saves time but also minimizes errors.
Integration with EHR systems
One of the key strengths of RCM services is their seamless integration with Electronic Health Record (EHR) systems. This integration ensures that billing and clinical documentation are synchronized, eliminating redundancies and ensuring accuracy.
Improved financial visibility
By optimizing RCM, healthcare providers gain insights into their financial health. Real-time analytics and reporting tools provide a clear picture of revenue streams, allowing informed decision-making.
Enhanced compliance
Compliance with healthcare regulations is non-negotiable. RCM optimization keeps providers up-to-date with ever-changing regulations, ensuring adherence to guidelines and mitigating compliance risks.
How streamlining RCM benefits healthcare providers?
As healthcare providers navigate the intricate landscape of patient care, administrative burdens become hefty. Optimizing the revenue cycle management process reduces these burdens.
The benefits of RCM optimization are clear and compelling—improved efficiency, reduced errors, and enhanced financial stability. Healthcare providers streamline operations and elevate the standard of care they deliver to patients. Here are other benefits of streamlining RCM to healthcare providers.
Improved efficiency
Time is a precious commodity in healthcare, and streamlining RCM offers a valuable gift—more of it. By automating tedious administrative tasks, healthcare providers reclaim hours once lost to paperwork.
Streamlined workflows
With optimized RCM, handling bills, claims processing, and documentation becomes easy. Staff can redirect their focus toward what truly matters—providing quality care to patients.
Automated accuracy checks
Through built-in algorithms and validation rules, healthcare providers can catch errors before they escalate. This proactive approach minimizes rework, saving time and resources.
Code compliance
Keeping up with ever-evolving coding regulations can be difficult. Healthcare providers should stay abreast of changes, ensuring claims are coded correctly and compliant with industry standards.
Financial stability
A stable financial foundation is essential for the growth and sustainability of healthcare providers. Streamlining the RCM process builds this stability by optimizing revenue streams and securing financial health.
Optimized revenue cycle
Healthcare providers should streamline the entire revenue cycle from claims submission to payment reconciliation. This increases revenue capture and minimizes revenue leakage.
Transparent insights
Through robust analytics and reporting, healthcare providers can clearly view financial performance. Providers can identify trends, track key metrics, and make data-driven decisions for long-term financial success.
Mitigated compliance risks
Non-compliance can spell disaster for healthcare organizations. Streamlining the RCM process ensures adherence to regulations, reducing the risk of audits, penalties, and reputational harm.
Conclusion
In healthcare operations, administrative tasks have always been a challenge. For healthcare providers seeking to streamline their administrative tasks quickly and efficiently, now is the time to explore the possibilities of RCM. PCH Health has provided end-to-end RCM solutions for over 30 years. We offer innovative and efficient services to create a vibrant landscape of options. With PCH Health's revenue cycle management solutions, healthcare providers can revolutionize their operations, ensuring a brighter, more efficient, and patient-centered future. Contact our experts today to discover how RCM solutions can transform your facility.
