
The 21st century has witnessed a profound transformation regarding mental health awareness. Once limited to whispers and cushioned tones, mental health conversations have taken center stage in our lives.
According to the recent Axios-Ipsos American Health Index, Americans perceive poor mental health as one of the biggest public health threats, ranking just behind obesity and the opioid epidemic. The report also revealed that nearly nine out of ten people consider mental issues as severe societal threats, surpassing concerns about access to firearms, COVID-19, or cancer.
Despite its severity, the treatment vastly differs from that of more traditionally perceived 'serious' illnesses. This discrepancy often leads to patients facing complicated and prolonged billing processes, further exacerbating their stress and hindering timely access to necessary care. Moreover, this discrepancy has equal effects on healthcare providers, leading to administrative challenges and potential delays in reimbursement.
About 1 in 25 U.S. citizens suffer from serious mental illness. Anxiety disorders, depression, bipolar disorder, Post-Traumatic Stress Disorder (PTSD), and schizophrenia are the top 5 mental disorders commonly found in the U.S. These facts make it crucial for mental health patients to get timely, quality care. At the same time, these facts emphasize the need for healthcare providers to receive accurate and timely reimbursements.
Accurate and timely medical billing requires special codes. Precisely documenting and coding mental, behavioral, and neurodevelopmental disorders can help capture members' health status and facilitate the continuity of quality patient care. Therefore, as a healthcare provider, you must take note of the minor details of ICD-10 coding for mental health. Read on to gain more insights into ICD-10 coding and improve your coding practices.
Medical coding for mental health conditions
Every passing year, millions of Americans experience symptoms of mental health conditions. And the number of people seeking care is only trending upward. A mental health diagnosis can significantly impact an individual's daily life and have a ripple effect across families, communities, and even economies. In addition, the impact of lengthy and complex medical coding adds to the challenges for patients and providers.
Medical coding for mental health involves accurately classifying mental health diagnoses and treatments using standardized code sets such as ICD-10 and CPT. This process ensures that mental health conditions are correctly documented and billed, facilitating effective communication between healthcare providers and insurance companies.
Accurate coding is essential for securing appropriate reimbursement, tracking treatment outcomes, and maintaining compliance with regulatory standards. Proper medical coding in mental health supports the financial health of healthcare practices and ensures patients receive the necessary care without administrative delays.
Coding for mental, behavioral, and neurodevelopmental disorders
ICD-10 code guidelines for behavioral health primarily include two categories: F and Z.
Category F (F01-F99):
These codes incorporate disorders of psychological development and include classification designations such as:
- With or without behavioral disturbance
- In remission
- With withdrawal
- Complicated or uncomplicated
These designations necessitate the provider's clinical judgment. The code explicitly associated with the designations should be captured only when documented by the provider, such as in cases of withdrawal or remission.
Category Z (Z00-Z99):
Z codes include different stress factors and social needs that can be a part of behavioral health conditions. These social determinants of health (SDOH) might possibly affect a patient's willingness or capability to follow their recommended treatment plan. Z codes represent particular symptoms a patient might encounter, but they don't signify a specific disorder, and the patient still might need warranted treatment.
What are ICD-10 codes?
ICD-10 (The International Classification of Diseases, 10th revision) is the standardized set of codes adopted by the Department of Health and Human Services (HHS) as instructed by the HIPAA Administrative Simplification guidelines. This system simplifies the reporting of diagnoses and enhances communication between healthcare entities.
Developed by the World Health Organization, ICD-10 contains thousands of diagnosis codes and their corresponding descriptions for all clinical disciplines. This uniform code set enables providers, insurance payers, and government agencies to consistently report diseases and conditions for tracking and reimbursement purposes.
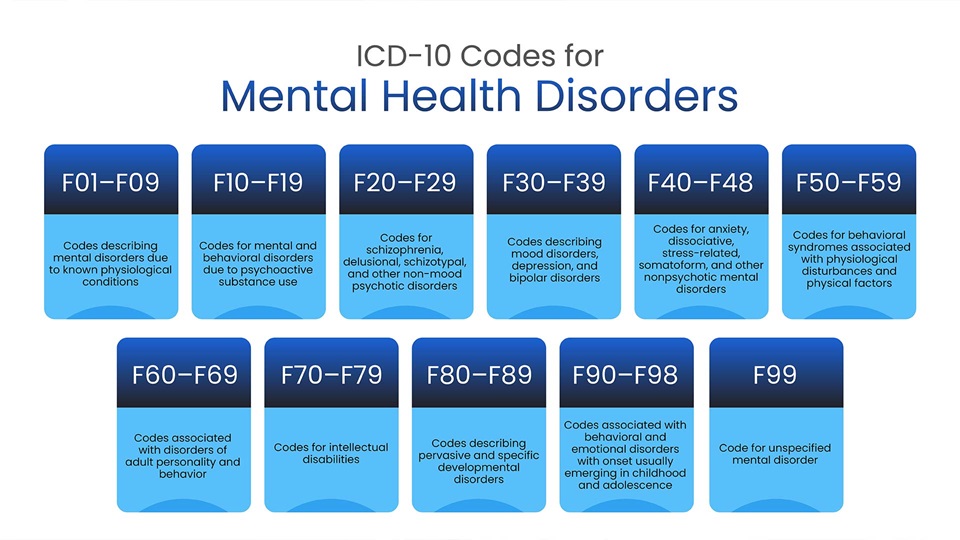
Typically, ICD-10 codes start with a single letter and are followed by three or more numbers. F codes are the most commonly used ICD-10 codes for mental health disorders. F codes are further divided into the following categories:
F01–F09: Codes describing mental disorders due to known physiological conditions
F10–F19: Codes for mental and behavioral disorders due to psychoactive substance use
F20–F29: Codes for schizophrenia, delusional, schizotypal, and other non-mood psychotic disorders
F30–F39:Codes describing mood disorders, depression, and bipolar disorders
F40–F48: Codes for anxiety, dissociative, stress-related, somatoform, and other nonpsychotic mental disorders
F50–F59: Codes for behavioral syndromes associated with physiological disturbances and physical factors
F60–F69: Codes associated with disorders of adult personality and behavior
F70–F79: Codes for intellectual disabilities
F80–F89: Codes describing pervasive and specific developmental disorders
F90–F98: Codes associated with behavioral and emotional disorders with onset usually emerging in childhood and adolescence
F99: Code for unspecified mental disorder
Best practices for mental health billing and coding
Maintain and manage proper documentation
Patients' data, including their demographics, medical history, and insurance information, is prone to updates and changes. These changes can affect the claims submission, compromising its accuracy. Any minor error in your claims can result in denials or rejections. Thus, ensuring that the patient's data is updated and relevant to the current scenario is crucial.
Check the patient's benefits
Verification of the patient's benefits should be the first and foremost stage before proceeding with the sessions. This process might seem unnecessary, but it is indisputable: It will keep the patients up-to-date with their medical plans, even if a change occurs.
Psychiatric Evaluation Codes vs. E/M Codes. Know the difference!
Healthcare providers delivering mental and behavioral health care may bill for psychiatric evaluations or even Evaluation and Management(E/M). The E/M codes incorporate the patient's medical history (illness history, social history, or family, and system reviews), examination (type of test or procedure that needs to be performed and nature of the illness), and medical decision-making (treatments documented, risk factors, and complexities associated with reviewed data).
The psychiatric evaluation codes are explicitly used for diagnostic assessment and can also fall under the E/M code umbrella. However, the coders must be knowledgeable about the codes to be used, which would result in clean claims.
Stay aligned with the insurance guidelines
Insurance companies have specific requirements for documentation and coding, which must be meticulously followed to ensure claims are processed smoothly. Accurate coding facilitates timely reimbursement and helps avoid claim denials and potential audits. By adhering to insurance guidelines, healthcare providers can ensure that patients receive the care they need without unnecessary financial or administrative burdens.
Stay on top of ICD-10 codes
Keeping up-to-date with ICD-10 codes is critical for accurate mental health documentation and billing. Regularly reviewing and understanding the latest codes and updates ensures that healthcare providers can correctly classify and report mental health conditions. This precision helps streamline the billing process, reducing claim denials and securing appropriate reimbursement. By staying on top of ICD-10 codes, providers can enhance the quality of patient care and maintain compliance with industry standards.
It's a wrap!
Accurate ICD-10 coding is of paramount importance in the field of mental health.
Mental healthcare providers can deliver the best care while optimizing reimbursement processes by adhering to specificity in coding, detailed documentation, regular training, leveraging technology, and collaboration with billing experts.
If you are looking for a mental health medical coding expert, you've come to the right place. At this point, you require a partner who can seamlessly resolve your coding queries and make technology integration seamless. That's where PCH Health comes into the picture.
Partnering with PCH Health can help you process clean claims without worrying about complex coding. Talk to our mental health medical billing and coding experts to learn more about our RCM services.
DISCLAIMER: The information on this site is for general purpose only and is not intended to serve as legal advice. Given the frequent changes in updates PCH Health cannot guarantee that all the information on this site is 100% accurate. Should you have specific question about any of the information on this site, feel free to write to us (marketing@pchhealth.global)
