
Medical coding compliance may not always make headlines, but it quietly holds the healthcare system together. Without it, claims go unpaid, audits accumulate, and systems collapse. So, why is it becoming increasingly difficult to stay compliant in 2025? Regulations keep changing. Coding logic keeps evolving. And payers are watching more closely than ever.
Hospitals, ambulatory surgery centers, and private practices all feel the pressure. Documentation requirements are stricter. Review cycles are faster. Errors, even small ones, now come with higher costs. So, how do you keep up and stay compliant, without slowing your teams down?
Here's what medical coding compliance really means, why it's critical to your revenue, and what it takes to get it right.
What Is Medical Coding Compliance?
Medical coding compliance involves ensuring that the codes used on claims accurately reflect the care that was actually provided. It’s not just about choosing the right ICD-10, CPT, or HCPCS codes. It’s also about following payer rules, government regulations, and documentation standards.
Every chart has to hold up under review. That means coders need clear provider notes, current code sets, and tools that help catch issues early. When teams stay aligned, coding becomes more consistent. And when the process is consistent, compliance gets easier.
Why Compliance Matters
When coding and compliance don’t work hand in hand, it shows up in all the wrong places. Claims get denied. Audits start stacking up. Payers lose trust. And teams spend more time fixing problems than doing their actual jobs.
In 2025, the pressure is higher. CMS has increased post-payment reviews. Commercial payers have automated parts of their claims review process. That means errors, especially recurring ones, get flagged faster, and the consequences can come quickly.
Here’s what’s at risk without a solid coding compliance plan:
- Revenue Delays: Even minor coding mistakes can lead to claim denials or underpayments.
- Legal Trouble: Incorrect billing can trigger violations under the False Claims Act.
- Increased Scrutiny: Once flagged, providers often face follow-up audits that can significantly slow down the process.
- Damaged Relationships: Repeated errors can erode trust with payers and cause long-term issues with reimbursement.
- Operational Drain: Teams end up chasing corrections, not revenue.
But when medical coding compliance is done well, the difference is easy to see:
- Claims move faster through the system.
- Denials slow down because the documentation aligns with the codes.
- Coders and auditors work more efficiently, with fewer surprises.
- Providers get paid accurately and faster.
- There’s more confidence across the board, from front-line staff to leadership.
Key Regulations and Guidelines
Different provider types follow different sets of rules. However, regardless of your specialty, certain regulations apply universally. In 2025, pay close attention to:
HIPAA Security Updates
The 2025 HIPAA updates have a significant impact on coding compliance. They streamline patient access to their records, reduce response times for requests, and introduce new protections for reproductive healthcare information.
Key changes include:
- Mandatory multi-factor authentication (MFA) for all ePHI access points
- Enhanced risk analysis requirements
- Stricter data security measurements
CMS Billing Guidelines
The latest CMS medical coding guidelines include updates to ICD-10-CM and CPT/HCPCS codes, revised E/M coding and documentation requirements, and increased scrutiny on modifier usage.
To be more specific:
- CMS has released a wide range of ICD-10-CM codes covering various conditions and diseases
- CMS is emphasizing stricter E/M coding and documentation requirements
- They have expanded telehealth coverage to include remote patient monitoring and AI-driven consultations
OIG (Office of Inspector General) Compliance Updates
- The recent updates focus on enhanced scrutiny of coding and billing practices in 2025, particularly in relation to global surgery coding and telehealth services.
- There will also be a push for stronger enforcement of accurate documentation, especially for telehealth, and a review of postoperative services to prevent overreporting.
- Additionally, the OIG is seeking increased funding to expand its investigations into fraud and abuse in Medicare, Medicaid, and the Children's Health Insurance Program.
AMA CPT Changes
- Effective January 2025, the American Medical Association (AMA) has released the 2025 CPT code set, which includes 270 new codes, 112 deletions, and 38 revisions.
- These changes are a testament to the advancements in medical technology, particularly in areas like genetic testing and digital medicine.
- Key updates include new codes for autografts, arthroplasty, and other surgical procedures within the Surgery section, as well as new telemedicine codes.
What Goes Into a Strong Coding Compliance Plan
A coding compliance plan is the foundation that keeps your documentation, billing, and audit practices consistent. It outlines your commitment to accurate coding, ethical billing, and regulatory alignment. It's more than a document—it's the structure behind every claim you submit.
An effective coding compliance plan needs to include:
- Defined roles and responsibilities for who oversees compliance and who manages risk
- Written policies that clarify how coding decisions should be made and documented
- Regular internal audits to check for patterns of risk or frequent mistakes
- Targeted training that keeps coders and providers informed about updates and documentation needs
- Incident response protocols for when issues are found, including how to correct and prevent them
- Technology documentation showing how tools like CAC or AI support accurate, compliant coding
When done right, your plan becomes a daily guide—not something you pull out during an audit, but something that actively reduces risk and confusion in your day-to-day work.
What a Compliant Coding Process Looks Like
It’s one thing to talk about compliance in theory, but what does it look like in day-to-day work? Here’s how a typical workflow should go when things are running right:
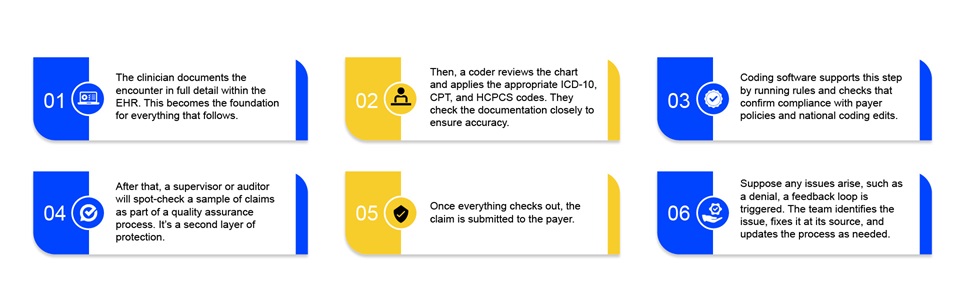
This workflow ensures accurate coding, clean claims, and that everyone is on the same page.
Best Practices for Staying Compliant
Even with a strong plan, compliance ultimately depends on execution. These best practices help organizations keep their plan active, not passive.
Invest in Continuous Learning
The only constant in the world of medical coding is change. To ensure your coders are equipped with knowledge of ever-evolving coding guidelines and standards, it is essential to invest in their continuous learning. This could be achieved by conducting regular training sessions and encouraging them to pursue certifications, such as Certified Professional Coder (CPC) or Certified Coding Specialist (CCS).
Conduct Regular Audits
One of the most effective ways to prevent denials is to conduct regular audits. Why? Because it helps in identifying errors, differences, and areas of non-compliance. With this knowledge, you can take corrective actions and ensure that this doesn't happen again. Relying on autonomous medical coding tools to conduct thorough audits for you could be extremely beneficial, as its AI algorithms can be trained to identify patterns and anomalies that may indicate fraudulent or abusive billing practices.
Strong Communication Channels
Effective communication between coders and healthcare providers is crucial for ensuring medical coding compliance. Why? Because it allows coders to request clarification on unclear documents and solicit feedback from providers. This back-and-forth communication helps coders better understand the context of treatments, diagnoses, and procedures, which in turn improves coding accuracy.
Leverage Latest Tools & Technology
In addition to investing in continuous learning, you should consider investing in the right medical coding automation software. Why? AI-powered coding systems leverage natural language processing (NLP) and machine learning (ML) to analyze large volumes of data and accurately translate them into standardized codes. Thus ensuring coding accuracy and reducing workload and turnaround times. It's a one-time investment that can yield double the ROI.
Create a Culture of Compliance
Fostering a culture that prioritizes coding compliance is utmost important for long-term success. It is an environment where every member of the healthcare team understands their role in upholding legal and ethical standards. A compliance-first culture begins with the organization's leadership, as when authority figures demonstrate integrity and adherence to compliance, employees are more likely to follow suit.
Tools That Make Compliance Easier
In 2025, you cannot expect coders to manage compliance alone, especially not with the volume and complexity of today's claims. The right tools make a big difference.
CAC software helps coders select the appropriate codes by analyzing the chart content. EHRs reduce manual errors by centralizing information. Audit dashboards help spot trends and fix recurring issues. Systems that update code sets automatically ensure your team is always using the most recent data.
But what about AI?
That's where platforms like PCH Health come in.
Our autonomous coding platform uses artificial intelligence, machine learning, and natural language processing to apply and validate codes based on the information in the chart. It handles CPT, ICD-10, HCPCS, and E/M codes across high-volume workflows. It also checks coding logic rules before claims are sent out, reducing denials before they occur.
The best part: It logs every decision.
So if you ever get audited, you have the full picture.
What Compliance Looks Like in Real Life
Think about your workflow. When a chart is coded, who is double-checking that the right modifier is used? How quickly do updates make it into your system? When was the last time you did an internal audit?
If your answers are fuzzy, you're not alone. That's why a structured compliance process matters.
Let's say a claim gets flagged during a payer review. If your audit trail is clean and the coding logic is sound, that claim is safe to make. If your process is unclear or if your tech missed something, it could result in delayed payment or worse.
What to Look For in a Medical Coding Compliance Tool
Not every solution fits every team. Here's what to prioritize:
- Speed: Can it handle high volumes?
- Accuracy: Does it catch issues early?
- Flexibility: Can it handle multiple specialties and workflows?
- Transparency: Are decisions well-documented?
- Support: Is the vendor responsive and familiar with regulatory changes?
Our platform, for example, supports over 43,000 encounters per hour. It scales across ASC and hospital workflows, supports coder validation, and adapts as rules evolve. That means more control, less confusion.
Curious to see how it works?
Schedule a personalized demo to discover how PCH Health fits into your compliance strategy.
FAQs
Q1) How can healthcare providers stop claim denials from coding mistakes?
A) To keep denials at bay, it is important to:
- Conduct regular coding audits
- Train your coders on the latest coding regulations and guidelines
- Have a clear communication channel between coders and clinicians
- Invest in the right tools and technologies
Q2) What’s the impact of the 2025 HIPAA rules on coding compliance?
A) The 2025 HIPAA updates have significantly impacted coding compliance. They improve patient access to their records, speed up request processing, and add new safeguards for data pertaining to reproductive healthcare.
Key changes include:
- Mandatory multi-factor authentication (MFA) for all ePHI access points
- Enhanced risk analysis requirements
- Stricter data security measurements
Q3) Why do coder certifications matter for compliance?
A) Certified coders = coding compliance. How? They bring in a wealth of knowledge on coding guidelines, regulations, and medical terminology. This allows them to assign every code with precision, which ultimately results in fewer denials.
