According to the American Medical Association, Prior Authorization (PA) is the process by which healthcare providers and physicians obtain advance approvals from a health insurance plan before delivering a particular service, procedure, device, supply, or medication to a patient to qualify for coverage.
Payers use prior authorization to review and approve certain medical services and medications before they are provided to ensure they are medically necessary and cost-effective.
Although the process primarily intends to save healthcare dollars, it often becomes a cost sink, consuming invaluable time, money, and resources. Errors, rework, and frustration impede the timely delivery of care, erode patient trust in their health plans, and create friction between payers and providers.
These inefficiencies contribute nearly $1 trillion in annual administrative costs to healthcare. However, effective measures can overcome these challenges and let the process do its job—reducing unnecessary costs and enhancing patient care efficiency.
Let's understand the process, its challenges, and ways to overcome them.
Understanding prior authorization in healthcare payers
John, a 45-year-old man, suffers from chronic back pain, and his doctor suggests an MRI scan to identify the underlying cause. Since MRI scans are expensive, John's healthcare provider must obtain prior authorization from his insurance company before proceeding.
Here are the steps involved in the prior authorization:
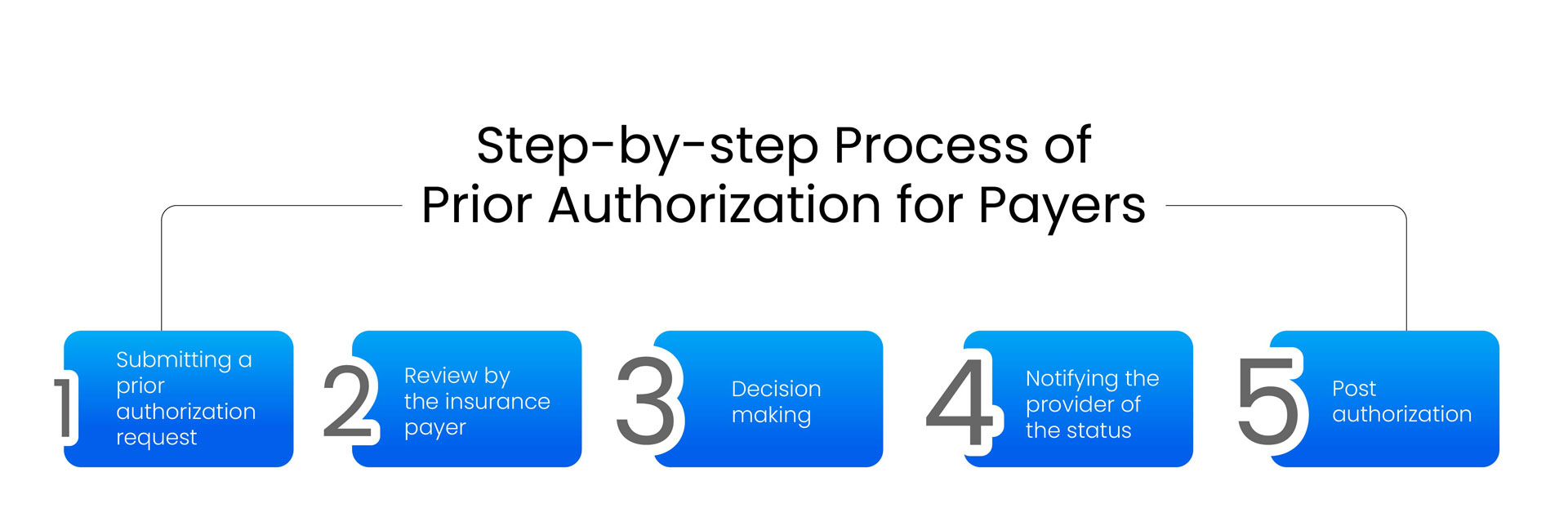
Submitting a prior authorization request
Physicians or healthcare providers prepare the necessary documentation, including the patient's medical history, symptoms, previous treatments, and the reason for the treatment. This information is submitted to the patient's insurance company through a prior authorization request form, either electronically or via fax.
Review by the insurance payer
A medical reviewer at the insurance company reviews the submitted documents to ensure all required information is provided. The insurance company's clinical team assesses whether the treatment is medically necessary based on the patient's condition and current medical guidelines.
Decision making
If the insurance company agrees that the suggested treatment is medically necessary, it issues an authorization number, which is communicated back to the physician. This approval means the company agrees to cover the cost of the treatment, subject to the policy terms.
If the payer determines that the treatment is not medically necessary, it denies the request and provides reasons for the denial. In our scenario, John's doctor can either appeal the decision or discuss alternative diagnostic methods.
Notifying the provider of the status
The insurance company notifies the physician or healthcare provider about the approval or denial. If approved, the authorization number and specific instructions are provided.
Post-authorization
With the authorization in hand, providers can schedule the treatment. The facility performing the care uses the authorization number to ensure that the service will be covered.
After the physician delivers care, the facility submits a claim to the insurance company using the authorization number, ensuring streamlined processing and payment.
In a nutshell, by understanding and efficiently navigating the prior authorization process, healthcare providers can secure necessary approvals, and patients like John can receive essential medical services without financial burden. PA helps reduce unnecessary costs, allows patients and providers to submit claims efficiently, and ensures treatment aligns with the current medical policies and guidelines.
Common prior authorization challenges
Here are some key findings from a survey conducted by the American Medical Association regarding prior authorization:
- 93% of physicians reported that obtaining prior authorization led to delays in patient care.
- 82% of physicians stated that prior authorization sometimes or often resulted in patients abandoning treatment.
- 24% of physicians reported instances where prior authorization requirements led to a patient's hospitalization.
- 2 in 5 physicians have staff dedicated solely to handling prior authorizations.
These facts highlight the significant impact of prior authorization on the quality of care and physicians' revenue, making it equally essential to streamline the process. Here are some common challenges of prior authorization

Manual processes
The primary burden in prior authorization is the extensive manual process it entails. The processing time for a prior authorization request by an insurance company varies based on factors like request complexity, therapy or drug type, and internal processes and workload. Decision times typically range from a few days to several weeks on average. Moreover, this manual process is slow, error-prone, and can cause significant treatment delays.
Poor provider & member experience
Poor provider and member experience is the second most significant challenge of the prior authorization process. The process itself has adverse effects on both members and healthcare providers, resulting in subpar experiences for both. The existing process frequently causes care delays, heightened administrative workload, and provider frustration.
Likewise, members may encounter delays in obtaining essential treatments or medications, leading to dissatisfaction and possible adverse health consequences.
Appeals and denials
Increased denials pose a significant challenge for healthcare payers. When payer organizations frequently deny authorization requests, they add to administrative burdens and strain relationships with healthcare providers.
The process of appealing denials consumes additional time and resources for both payers and providers, leading to delays in patient care and potential disruptions in treatment plans.
Provider guidelines
Increased provider guidelines pose a significant challenge to the prior authorization process. As the guidelines become more complex and stringent, healthcare payers must invest more resources in training staff, updating systems, and ensuring compliance.
Managing a wide array of guidelines from various providers can be overwhelming, leading to confusion, errors, and delays in processing prior authorization requests. Moreover, frequent changes to guidelines require constant monitoring and adaptation, further adding to the administrative burden.
Lack of interoperability
The absence of interoperability among healthcare systems and insurance companies is a significant burden in prior authorization. Without standardized codes and communication protocols, exchanging information between providers and payers becomes challenging. This lack of interoperability results in inefficiencies, delays, and added complexity to the prior authorization process.
Ways to overcome prior authorization challenges
Automation
Implementing automated prior authorization software eliminates manual paperwork and reduces errors. Moreover, it helps process prior authorization requests electronically, saving time and improving accuracy.
Electronic data exchange
Establishing electronic data exchange between providers and insurance companies enables seamless communication and faster decision-making. Real-time verification of patient eligibility reduces the need for manual intervention.
Transparency in requirements and timelines
Insurance companies should offer healthcare providers clear and transparent guidelines regarding prior authorization requirements and timelines. This transparency enables providers to prepare and submit accurate requests, minimizing the risk of unnecessary denials or delays.
Outsourcing services
Healthcare payers can opt to outsource prior authorization tasks to specialized companies or vendors. This approach can ease the administrative burden on in-house staff, as external service providers are adept at navigating the complexities of prior authorization. They ensure accurate and timely processing of requests, thereby streamlining the process and improving efficiency.
Investment in technology infrastructure
Robust technology infrastructure must be prioritized to address the lack of interoperability. This involves implementing electronic health record (EHR) systems capable of seamlessly integrating with insurance company platforms, facilitating efficient data exchange.
Conclusion
Understanding the complexities of prior authorization is essential for healthcare payers to navigate this crucial aspect of the healthcare system effectively.
Challenges such as manual processes, increased guidelines, and lack of interoperability can impede the efficiency of prior authorization, leading to delays and frustration for both providers and members. However, with the right strategies and technological investments, payers can overcome these hurdles and streamline the prior authorization process.
At PCH Health, we understand the importance of streamlining prior authorization for insurers. Our innovative solutions leverage advanced technology to automate and optimize the prior authorization workflow. Talk to our experts to learn more about our services.