What is medical coding?
Medical coding is a process of applying standard alphanumeric codes to the diagnosis and procedures offered to patients. Medical coding happens every time a patient receives service from a healthcare provider. When a patient visits a clinic, the provider reviews the patient's medical history and complaint, decides on the treatment to offer, and documents the visit. This documentation is critical for a patient's ongoing treatment and for healthcare providers to get paid. It involves converting a patient's medical information, such as:
- Diagnosis
- Procedures
- Medical service information
- Necessary medical equipment
Medical coders apply proper ICD, CPT, or HCPCS codes during billing.
Private or government insurance companies must pay this claim.
Types of medical code sets
Medical coders apply proper ICD, CPT, or HCPCS codes during billing. There are majorly three types of medical coding sers.
ICD (International Classification of Diseases)
The WHO (World Health Organization) created these ICD codes that are now used internationally. The classification system is used primarily for data collection and health recording. These codes can classify diseases, symptoms, causes of death, and illnesses.
CPT (Current Procedural Terminology)
CPT codes identify surgical, diagnostic, and medical services & procedures. The AMA (American Medical Association) developed these medical codes, which include emerging technologies, clinical labs, methods, and contemporary medical practices.
HCPCS (Healthcare Common Procedure Coding)
The CMS (Centers for Medicare and Medicaid Services) developed this coding system to aid claim processing for private and government payers. Coders use them to note medical products, procedures, services, and supplies.
Medical coding ensures that RCM is done seamlessly and claims are processed correctly. It is also used for patient records and research purposes.
Every medical code tells payers, providers, and researchers the exact procedures, diagnoses, and services offered. It universally qualifies patient visits and makes healthcare provider notes less abstract for payers and future healthcare treatment.
Medical codes also tell the payers about
- Medical necessity for services, treatment, or the supplies offered to the patient
- Any unusual medical condition or circumstances that affect those services and treatments
Medical coders work closely with payers, providers, and management. They review a particular discipline and skills like problem-solving, detective work, and scholarship. The medical coders process multiple claims daily and must be as specific as possible when collecting payment for a particular service rendered.
What is a clinical coder?
The clinical coder is the person who converts patient records into universally accepted medical codes. These codes simplify healthcare communication, data analysis, and medical billing. The clinical coder also ensures that:
- Healthcare providers are paid appropriately
- Claims are processed correctly
- Patients receive the benefits
A clinical coder also:
- Connect patient care and claim processing
- Support healthcare providers' financial health
- Contribute to public health and medical research
The data generated through clinical coding helps in research, policy-making, and public health monitoring.
Importance of medical coding
Medical coding is important as it ensures timely payments to healthcare providers and prevents patient billing disputes. Accurate coding minimizes billing errors and is crucial to revenue cycle management. Providers are reimbursed based on the codes and modifiers submitted for each patient’s services, diagnoses, or equipment. Both government and private payers use these standardized codes to process claims efficiently.
Coding regulations set by payers and organizations like the CMS provide clear standards that help practices minimize errors, ensure compliance, and avoid legal risks. Here is what a streamlined medical coding process can do for healthcare providers.
Enhances patient care and safety
Medical codes track disease prevalence, outcomes, and treatment efficacy. This data is used for public health monitoring and research, leading to better healthcare policies and practices.
Medical coding also ensures that patient records are
- Up-to-date and comprehensive
- Critical for continuous care
- Effective care coordination
- Well-researched and available in public health data
When patients transition between providers or levels of care, it’s critically important that their medical history is accurately communicated. Medical coding ensures a clear, standardized record that helps new providers quickly understand the patient’s history, allowing appropriate care.
In complex cases involving multiple specialists, coding enhances coordination among healthcare teams by providing consistent information to all providers, reducing the risk of errors.
Supports healthcare analytics and decision-making
Data is the foundation for robust analytics in today's tech-driven healthcare environment. Medical codes serve as the raw data that powers various analytical tools, enabling providers to identify trends, optimize resource allocation, and enhance the quality of care. Using this information, healthcare providers can:
- Detect areas for improvement
- Refine treatment protocols
- Enhance the quality of care provided
Healthcare providers can also find patient populations, treatment outcomes, and resource utilization by analyzing coded data. This information is vital for strategic planning and improving care delivery.
Hospitals and clinics can use coding data to understand which services are most in demand, allowing them to allocate resources more efficiently.
Example: A surge in specific diagnoses might prompt a hospital to increase staffing or invest in specialized equipment.
Impact of incorrect medical coding
Incorrect coding (down coding) leads to improper payments, affecting the financial health of providers. On the other hand, upcoding can lead to audits and potential penalties.
Medical coding examples
Medical coding examples are numerous and change with different procedures and treatments. Here are a few examples that would help you understand medical coding better.
ICD-10-CM
E11.9
This code represents Type 2 diabetes mellitus without complications. The "E" indicates it's an endocrine, nutritional, and metabolic disease; the numbers further specify the exact condition.
J20.5
This code represents acute bronchitis caused by a respiratory syncytial virus. "J" codes cover diseases of the respiratory system.
CPT
99203
This code is used for an office or other outpatient visit to manage and evaluate a new patient. It requires a detailed history, detailed examination, and low-complexity medical decision-making.
45380
This code represents a colonoscopy with a biopsy. The CPT code 45380 specifies that a biopsy was performed during the colonoscopy.
HCPCS
EO135
This code represents a standard walker. HCPCS code like this is often used for durable medical equipment (DME).
G0008
This code is used to administer the influenza virus vaccine. HCPCS codes include not only durable medical equipment but also services and procedures not covered by CPT.
Modifiers
LT
Modifiers like LT (left side) and RT (right side) are used with CPT codes to provide additional information about the procedure. In this case, LT would indicate that the surgery was performed on the patient's left arm.
53
The 53 modifier indicates that the procedure was discontinued due to unforeseen circumstances, such as patient instability.
Examples of specialty medical coding
Surgical
A patient undergoes a laparoscopic appendectomy.
ICD-10-CM Code: K35.80 (Acute appendicitis without perforation or abscess)
CPT Code: 44970 (Laparoscopy, surgical, appendectomy)
Radiology
A patient receives an MRI of the brain without contrast.
ICD-10-CM Code: R51 (Headache, to indicate the reason for the MRI)
CPT Code: 70551 (MRI of the brain without contrast)
Emergency room
A child presents with a laceration to the forehead.
ICD-10-CM Code: S01.81XA (Laceration without foreign body of another part of the head, initial encounter)
CPT Code: 12011 (Simple repair of a laceration on the face, less than 2.5 cm)
Bundle services medical coding example
A patient receives an injection for knee osteoarthritis, followed by physical therapy.
CPT Code: 20610 (Arthrocentesis, aspiration, and/or injection; major joint or bursa, with or without ultrasound guidance)
CPT Code: 97110 (Therapeutic exercises to develop endurance, strength, range of motion, and flexibility)
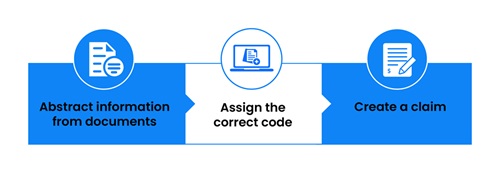
Medical coding process flow
The medical coding process flow is the steps medical coders follow to submit claims. It ensures compliance, aids in optimizing reimbursements, impacts patient care and helps in organizational sustainability. Here is the medical coding process flow.
Patient encounter and documentation
Documentation and patient encounters are the foundation for accurate RCM. When a patient visits a clinic, the healthcare provider records all required details, such as symptoms, diagnoses, procedures, and any treatments provided.
Medical record review
Medical coders then review the patient's medical records. They carefully examine the provider's notes, lab results, radiology reports, and other documentation to extract the relevant information.
Code assignment
After this, medical coders assign specific codes and modifiers to the collected information, i.e., the patient's diagnosis, procedures, and other relevant healthcare services. These codes are standardized and come from ICD-10, CPT, and HCPCS coding systems.
Claim preparation
Once the medical codes and modifiers are assigned, they are used to prepare claims that will be submitted to private payers, Medicare, or Medicaid. Accurate claims preparation helps healthcare providers receive reimbursements for the services rendered.
Claim submission
With all assigned codes, the claim is submitted to the relevant payer, typically done via print and mail or electronically through a clearing house that checks for basic errors before forwarding the claim to the payer.
Payer review
Once the payer receives the claim, they review its accuracy, completeness, and adherence to compliance and guidelines. This review determines whether the claim will be fully reimbursed, partially reimbursed, or denied.
Payment or denial
If the claim is approved, the insurance company pays based on the contracted rates for the coded services. If the claim is denied, it must be corrected and resubmitted. Providers can even appeal the denial.
Reporting and follow-up
Finally, the claim status (whether paid or denied) is documented, and any necessary follow-up actions are taken. This may include managing denials, making corrections, or appealing decisions to ensure the provider is adequately compensated.
Understanding medical coding codes
Understanding medical coding codes is crucial for healthcare providers and medical coders to code and avoid errors seamlessly. Medical codes create consistency and uniformity across healthcare documentation and billing. Without these, interaction between patients, payers, and providers would become chaotic.
Major types of medical coding systems
Here are the major types of medical coding systems used in RCM. Each set of codes serves a distinct purpose and is used in specific scenarios.
ICD codes
The ICD code set, maintained by the WHO, is one of the world's most widely used coding systems. Currently, the ICD-10 version is in use, with plans for ICD-11.
ICD-10-CM
This version is used for diagnosing patients and is the standard for documenting diagnoses across all healthcare settings in the United States. The "CM" stands for clinical modification, a U.S.-specific adaptation of the ICD-10 code set.
ICD-10-PCS
This set is explicitly used for inpatient hospital procedures. The "PCS" stands for procedure coding system and is used to report surgical procedures performed in hospitals.
ICD codes provide a comprehensive way to describe diseases, conditions, and injuries, vital for treatment and billing purposes.
Example: A simple headache is coded as R51 in ICD-10, while a more complex diagnosis like type 2 diabetes with complications is coded as E11.65.
CPT codes
CPT codes are primarily used to document medical, surgical, and diagnostic services. These codes are divided into three categories:
Category I: These codes represent procedures and services widely performed and accepted by medical professionals.
Example: A primary office visit for a new patient might be coded as 99202.
Category II: These codes are optional and are used for performance measurement, tracking, and quality improvement.
Category III: These codes represent emerging technologies, services, and procedures yet to be widely adopted.
CPT codes are essential for billing purposes. They tell the insurance company what service was provided, enabling the provider to be reimbursed appropriately.
HCPCS codes
HCPCS codes are divided into two levels:
Level I: This is the same as CPT codes and includes codes for services and procedures.
Level II: These codes cover supplies, equipment, and other services not included in CPT codes, such as ambulance rides, prosthetics, or durable medical equipment (DME).
HCPCS codes are essential for Medicare and Medicaid billing, as they include codes not found in the CPT system.
Medical coding vs medical billing, what’s the difference?
Understanding medical coding vs medical billing difference helps healthcare providers to streamline their RCM. Though medical coding and billing are connected within the healthcare revenue cycle, they are different. Coding focuses on precise documentation, billing manages the financial aspect of the RCM.
Medical coding involves translating diagnoses, procedures, and services into standardized codes. Coders analyze clinical documentation and assign the appropriate codes to ensure accurate medical records. It is crucial for tracking health trends, supporting clinical research, and ensuring compliance with regulations.
Medical billing uses the codes provided by medical coders to prepare and submit claims for reimbursement. Billers ensure that healthcare providers receive accurate payment by managing claim submissions, processing payments, and handling claim denials or rejections.
Specialty coding
Specialty medical coding refers to the practice of assigning medical codes that are specific to certain medical specialties or fields of healthcare. It requires a deep understanding of the exact medical terminology, procedures, and treatments associated with a particular area of healthcare.
Medical coding is a big cluster divided into smaller clusters of specialty coding. Each specialty's coding needs and complexity are different, and medical coders must understand this.
Specialty coding is not just about translating clinical documentation into codes; it's about doing so with precision and expertise that reflects the complexity of specialized medical care. This level of detail is crucial because it directly impacts the accuracy of billing, the reimbursement process, and an organization's overall financial health.
Why is specialty medical coding necessary?
Specialty medical coding is necessary because it helps healthcare providers with following:
Accurate reimbursement
Errors in coding can lead to significant financial losses, either through underpayment or claim denials. Specialty coders, with their in-depth knowledge, help prevent these errors. They ensure accurate claim submission and reimbursement.
HIPAA compliance and avoidance of audits
Healthcare providers are subject to stringent regulations and frequent audits. Accurate specialty coding helps ensure compliance with these regulations, reducing the risk of audits and the potential coding error penalties.
Enhanced patient care
Specialty coders maintain comprehensive and precise patient records, supporting better patient care. Medical codes provide a clear and complete medical history that can be used to make informed decisions about ongoing and future care.
Optimizing the revenue cycle
Specialty medical coding ensures that claims are processed efficiently, reducing the reimbursement time. It maintains the financial stability of healthcare organizations, allowing them to provide high-quality care to their patients.
Challenges in specialty medical coding
Specialty medical coding comes with a set of challenges. It requires coders to have advanced knowledge and skills beyond general coding practices.
Complexity of procedures and diagnoses
Specialized fields often involve highly complex procedures and diagnoses that require precise documentation. Misunderstanding or misapplying these codes can lead to significant billing errors.
Constantly evolving medical knowledge
Medical knowledge and technology are continuously growing, particularly in specialized fields. Coders must stay up-to-date with the latest developments, including new procedures, treatments, and corresponding codes. It requires ongoing education, training, and access to the latest coding resources and tools.
Navigating multiple coding systems
Specialty medical coders must often navigate multiple coding systems. Each system has its rules and guidelines, varying depending on the specialty. Coders must be able to apply these systems accurately to ensure correct billing and reimbursement.
High stakes and pressure
Errors can significantly impact the cash flow of healthcare providers. Specialty coders may face pressure to code quickly and accurately, particularly in high-volume specialties where many claims are processed daily, requiring expertise and the ability to work efficiently under pressure.
Specialty medical coding in different fields
Medical coding for different specialties is different. Healthcare providers need to have knowledge of these to ensure compliance and prompt reimbursement. Here are the specialty medical coding in various fields.
Oncology
Oncology coding involves assigning codes for cancer diagnoses, treatments, and procedures. It includes everything from chemotherapy and radiation therapy to complex surgical procedures. Oncology coders must also be familiar with the specific codes used for various types of cancer and the stages of the disease, as these factors can impact billing and reimbursement.
Orthopedics
Orthopedic coding covers a wide range of procedures related to the musculoskeletal system, including fracture repairs, joint replacements, and spinal surgeries. Orthopedic coders must understand the specific terminology used in this field, the various procedures, and their corresponding codes.
Dermatology
Dermatology coding involves documenting and billing a wide range of skin-related procedures, from biopsies and excisions to laser treatments and cosmetic procedures. Dermatology coders must be familiar with the specific codes used for different skin conditions and treatments and the guidelines for coding cosmetic procedures, which are not covered by insurance.
What is physician coding?
Physician coding involves translating the medical services doctors provide into standardized codes that can be used for billing purposes. These codes represent everything from patient diagnoses to procedures performed during a medical visit. The physician coding process must be precise because these codes are the foundation upon which insurance claims are submitted and payments are received.
What is HIM coding?
HIM coding translates healthcare diagnoses, procedures, medical services, and equipment into standardized codes which are used for billing, insurance claims, statistical analysis, and compliance with healthcare regulations. HIM professionals ensure these codes accurately reflect patients' care, supporting clinical and administrative functions within healthcare organizations.
What is pharmaceutical coding?
Pharmaceutical coding is assigning standardized codes to medications and related healthcare products. These codes are used for claims, billing, and inventory management.
The building blocks: NDC, HCPCS, and CPT codes
The NDC (National Drug Code) is the cornerstone of pharmaceutical coding in the United States. It's a unique 10-digit, 3-segment number that identifies the label, product, and trade package size. The NDC is crucial for tracking and billing medications across healthcare.
HCPCS codes are used alongside NDCs, mainly for billing Medicare and Medicaid. These
alphanumeric codes cover a wide range of services, including pharmaceuticals.
Example: J-codes within the HCPCS system are specifically designated for drugs that are typically not self-administered, such as chemotherapy or immunotherapy agents.
Although CPT codes are more commonly associated with medical procedures, they sometimes include pharmaceutical codes, particularly in drug administration scenarios.
Challenges in pharmaceutical coding
One of the biggest challenges in pharmaceutical coding is keeping up with the ever-evolving landscape of drug formulations, dosages, and delivery methods. New drugs are constantly entering the market, each requiring precise coding. Drug pricing and reimbursement policy changes can complicate the coding process, necessitating frequent updates to coding systems.
Another challenge is the complexity of coding for combination therapies, where multiple drugs are administered together. Coders must ensure that each therapy component is coded accurately to avoid reimbursement issues.
The role of technology in specialty medical coding
Modern technology has improved the efficiency and accuracy of specialty medical coding. Computer-assisted coding (CAC) and autonomous coding use AI & natural language processing to analyze clinical documentation and suggest appropriate codes.
Electronic health records (EHRs) also play a crucial role in specialty coding by providing coders easy access to detailed clinical documentation. EHRs can help ensure that coders have all the information they need to assign accurate codes, reducing errors and improving the efficiency of the coding process.
Medical coding software
Medical coding software is a tool that helps healthcare providers code faster and efficiently. Investing in the right medical coding software goes beyond simply adopting a new tool—it’s about strategically enhancing your workflow. In RCM, the efficiency of medical coding software is vital. Healthcare providers can streamline operations, reduce claim denials, and improve cash flow by incorporating real-time updates and analytics.
The right software minimizes coding errors, speeds up claim submissions, and ensures compliance with the latest standards. To maximize its impact, customization, comprehensive training, and ongoing evaluation are essential, ensuring the software adapts to your specific needs and drives operational success.
The evolution of medical coding software
Medical coding software has come a long way from its rudimentary beginnings. Initially, coding was a manual, labor-intensive process with numerous errors. Today, medical coding solutions leverage artificial intelligence and machine learning to streamline processes, enhance accuracy, and improve efficiency.
Key benefits of modern medical coding software
Enhanced accuracy
Medical coding software utilizes advanced analytics and AI to minimize errors and correctly apply codes. It reduces claim denials and ensures compliance with ever-evolving coding standards.
Increased efficiency
Automation coding accelerates claim submissions and reduces the time spent on manual entry. This efficiency translates into faster reimbursements and improved cash flow.
Real-time updates
The medical coding landscape is constantly evolving with new codes and regulations. Cutting-edge software offers real-time updates, ensuring your coding practices align with the latest standards and requirements.
Integrated analytics
AI coding software comes with robust analytics capabilities. These tools provide insights into coding practices, identify trends, and highlight areas for improvement.
Compliance and risk management
Compliance with regulations such as ICD-10, CPT, and HCPCS is critical. Autonomous coding helps organizations stay HIPAA-compliant, reducing the risk of audits and penalties.
Tips to implement medical coding software
Medical coding software must seamlessly integrate into your organization's workflow. Here are a few to implement medical coding software efficiently:
Customization
Choose a medical coding software that can be tailored to meet your organization's specific needs. Customization ensures that the tool aligns with your coding practices and operational requirements.
Training and support
Invest in comprehensive training for your coding staff. Adequate training ensures that your medical coding team can fully leverage the software's capabilities and maximize its potential benefits.
Continuous evaluation
Assess your coding software's performance regularly. It includes monitoring its impact on efficiency, accuracy, and overall revenue cycle performance.
Medical coding systems
Medical coding systems are standardized codes used to represent medical diagnoses, procedures, and services. These codes facilitate the translation of complex medical terms into a structured format that can be easily understood and processed by healthcare providers, insurers, and other stakeholders. The primary coding systems include ICD, CPT, and HCPCS.
Medical coding systems are standardized codes used to represent medical diagnoses, procedures, and services. These codes facilitate the translation of complex medical terms into a structured format that can be easily understood and processed by healthcare providers, insurers, and other stakeholders. The primary coding systems include ICD, CPT, and HCPCS.
Why are medical coding systems important?
Medical coding systems are important as they ensure that healthcare providers are accurately reimbursed for their services. Proper coding reduces billing errors and claims denials. Accurate coding provides valuable data for healthcare research, policy-making, and quality improvement initiatives. This data helps track disease prevalence, treatment outcomes, and healthcare utilization trends.
Coding systems help ensure compliance with healthcare regulations and standards. They facilitate reporting health information for regulatory purposes and support adherence to payer requirements. Medical coding systems enable seamless communication between healthcare systems, such as electronic health records, RCM billing systems, and insurance platforms.
Challenges in medical coding systems
Medical coding systems come with their own sets of challenges. Coding errors can lead to claim denials, incomplete reimbursement, and compliance issues. The massive volume of codes and the complexity of coding rules can be overwhelming. Coding professionals must continually educate and train themselves to keep up with updates and changes to coding systems.
Here are a few of the challenges in medical coding systems:
- Ensuring accuracy and consistency in coding practices
- Maintaining healthcare data integrity
- Ensuring compatibility and interoperability between systems
Medical coding certification
Medical coding certification is a credential for healthcare coding that shows the professional knowledge of a medical coder. It demonstrates that the person has learned a specific medical coding system. It is crucial for those looking to excel in this field. Medical coding certification gives you the following:
Professional Credibility
Certification validates your expertise and knowledge in medical coding, distinguishing you from non-certified professionals. It demonstrates your commitment to the field and adherence to industry standards.
Career Advancement
Certified medical coders enjoy better job prospects and higher salaries than their non-certified counterparts. Certification can also open doors to advanced roles and specialized areas within healthcare coding.
Industry Recognition
Certification from a recognized body can enhance your reputation and credibility within the healthcare industry. It informs employers and colleagues that you possess accurate and compliant coding skills.
Continuous learning
The certification process involves rigorous training & examination, ensuring you stay updated with the latest coding practices, regulations, and technology.
Types of medical coding certifications
There are different types of medical coding certifications, and if you are planning to become a medical coder, you should know them.
Certified Professional Coder (CPC)
The AAPC (American Academy of Professional Coders) offers the CPC certification as one of the most widely recognized credentials in medical coding. It covers various coding topics, including CPT, ICD-10, and HCPCS codes.
Certified Coding Specialist (CCS)
The CCS certification, provided by the American Health Information Management Association (AHIMA), focuses on coding and classification systems for hospitals and other healthcare facilities. It emphasizes inpatient coding and healthcare data management.
Certified Coding Specialist – Physician-based (CCS-P)
Also offered by AHIMA, the CCS-P certification is designed for professionals working in physician-based settings. It covers outpatient coding, including CPT, ICD-10, and HCPCS codes.
Certified Inpatient Coder (CIC)
This certification, offered by AAPC, is tailored explicitly for coders working in inpatient settings. It focuses on ICD-10-CM and ICD-10-PCS coding.
Certified Outpatient Coder (COC)
The COC certification, also from AAPC, is geared towards coders working in outpatient settings. It covers CPT, ICD-10-CM, and HCPCS Level II codes.
Steps to achieve medical coding certification
Here are the steps to achieve medical coding certification. These steps help to simplify the journey of complex medical coding.
Education and training
Enroll in an RCM medical coding training program that aligns with your certification goals. Many programs offer courses specifically designed to prepare you for certification exams. Ensure the medical coding program is accredited and covers essential principles and practices.
Gain experience
While not always required, practical experience in medical coding can enhance your understanding and improve your performance on certification exams. Consider internships or entry-level positions to gain hands-on experience.
Prepare for the exam
Utilize study guides, practice exams, & other resources to prepare for the certification exam. Focus on key areas such as coding guidelines, medical terminology, anatomy, and billing processes.
Register and take the exam
Once you feel prepared, register for the certification exam through the relevant certifying body. Follow their guidelines for exam scheduling and preparation.
Maintain certification
After achieving certification, stay current with continuing education requirements to maintain your credentials. It may involve completing additional training or professional development activities.
DISCLAIMER: The information on this site is for general purposes only and is not intended to serve as legal advice. Given the frequent changes in updates, PCH Health cannot guarantee that all the information on this site is 100% accurate. Should you have specific questions about any of the information on this site, feel free to write to us (marketing@pchhealth.global)