
In the complex world of healthcare, optimized revenue cycle management is crucial for faster and complete reimbursements. Healthcare providers must streamline their medical billing and coding process to maintain compliance, improve patient satisfaction, and ensure timely reimbursement. This comprehensive guide covers the fundamentals, challenges, best practices, and more, to help you master medical billing and coding.
What is medical billing?
Medical billing includes submitting and following up on claims with payers to receive payment for services rendered. Medical billers translate healthcare services into claims and send them to payers. Medical billing consists of professional and institutional billing, which, if done appropriately, can optimize revenue performance for healthcare providers.
Professional billing is the process of generating claims for physicians, non-institutional healthcare providers, or suppliers. It covers inpatient and outpatient medical services. Institutional billing includes charges related to administrative interventions during a patient’s stay, such as hospital beds or skilled nursing facilities. It includes radiology or laboratory services and the supplier or equipment used. Constant follow-up needs to be taken from insurance companies to ensure maximum reimbursement for the services offered to the patients.
What are the 10 steps of medical billing?
Medical billing is the backbone of healthcare RCM. It involves multiple steps, from the initial patient registration to the final payment receipt. Practices must do it right to ensure healthy cash flow and streamlined practice growth.
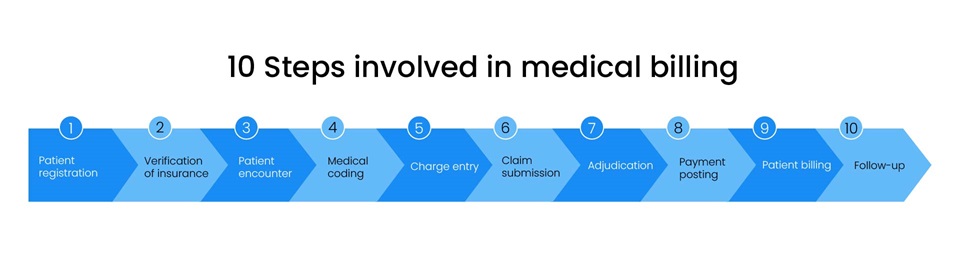
Patient registration
Patient registration is a vital step in healthcare RCM. It refers to recording and collecting essential medical information, financials, and demographics about the patient. It begins when a member schedules an appointment. The collected information is verified during registration, ensuring the claims will be processed correctly.
Patient registration is the first step and the point of contact between a healthcare provider and a patient. It involves completing various documents and forms, including insurance verification forms, patient intake forms, financial responsibility agreements, and consent forms. Patient registration is vital as it identifies patient identity, checks for insurance and eligibility, validates patient allergies and history, is used for medical billing, and can build robust communication between patient and provider.
Verification of insurance
Before offering services or treatment, the healthcare provider verifies insurance eligibility and benefits to understand the covered services and the patient's responsibilities regarding copays and deductibles. It is a step-by-step approach for healthcare providers to check if payers will pay for services proposed to patients. Insurance verification can not be skipped as it would leave healthcare providers with denied or unpaid claims. It consists of four steps:
- Receiving patient schedule
- Verifying payment extent with payers
- Connecting with patients for missed payment
- Keeping the billing step updated with patient eligibility details
Patient encounter
During the patient's visit, the healthcare provider documents the services, including diagnoses, treatments, and any procedures performed. It is vital to document this information as medical coders use it to assign appropriate codes to the process and diagnosis. Medical billers use this information to create claims. Errors in patient encounters might lead to errors in the claim submission process.
Medical coding
Medical coding is the most critical step in the billing cycle. Here, AAPC/AHIMA-certified specialty medical coders translate the documented services into standardized CPT/ICD codes, which describe the diagnoses and procedures in a universally accepted format. Medical coders need to ensure that services are appropriately bundled and there are no up or down coding instances. Medical coding involves using medical codes and being responsible for appropriate documentation. Payers check for medical codes to process reimbursements, and errors while coding might result in payment loss for healthcare providers.
Charge entry
Charge entry refers to accurately recording and posting charges for medical procedures and services offered to patients. Appropriate charge entry can avoid errors like over-billing or under-billing of patients. It helps healthcare providers to stay compliant and avoid delayed payments. In the charge entry process, RCM experts use medical codes to create a bill, known as a claim. It includes a breakdown of the services offered and their associated costs. Medical billers and coders sometimes collaborate to create a superbill. Superbills are sent to payers or patients according to the patient's insurance coverage.
Claim submission
Post charge entry, claims are submitted to the payers. Claim submission is vital as it determines reimbursement for healthcare providers. Clean claim submission ensures that your A/R days are minimum and your revenue cycle is optimized. Claim submission can be done on paper or electronically using tools offered by RCM service providers like PCH Health. Electronic submission is more common and efficient as it saves time and resources.
Adjudication
Once the claim is submitted, payers validate the claim and check whether the patient's insurance plan covers the services. They then decide the reimbursement amount and what portion, if any, the patient owes. Claim adjudication consists of majorly four steps:
- At the initial review, payers check the basic claim details, such as name, diagnosis, location, and service codes.
- In automatic review, insurance companies scan their systems in detail to check for prior authorization, the process's medical necessity, and the treatment's effectiveness.
- In the manual review step, insurance companies quickly scan the claims to make a final decision. Manual review is also performed on submitted expensive and complex claims.
- Once the manual and automated review is done, payers come up with a decision of payment, which is payment in full, partial payment, or payment denials.
Payment posting
Once the claim is processed, payers pay healthcare providers. The payment details are then posted to the patient's account. The payment process should be accurate as it directly affects healthcare providers' revenue cycles. It gives you clean insight into payments, smoothens the medical billing and payment collection process, and offers opportunities to increase revenue.
Patient billing
If there is a balance after the insurance company has paid its portion, the patient is billed for the remaining amount. It is vital to provide patients with a clear bill, multiple payment options, and explanations of their payments. Appropriate patient billing results in an increase in patient satisfaction and on-time payments.
Follow-up
In case of claim denials or incomplete payment, follow-up actions are taken to resolve the issues, including resubmitting claims or appealing denials. While appealing for denials, healthcare providers can also include comments or notes on superbills to justify the necessity of a particular treatment, service, or drug. Prompt follow-up results in faster payment and reduces the A/R cycle.
What are the most common medical billing and insurance terms?
Understanding the terminology used in medical billing is crucial for navigating the billing process efficiently. Here are some standard terms:
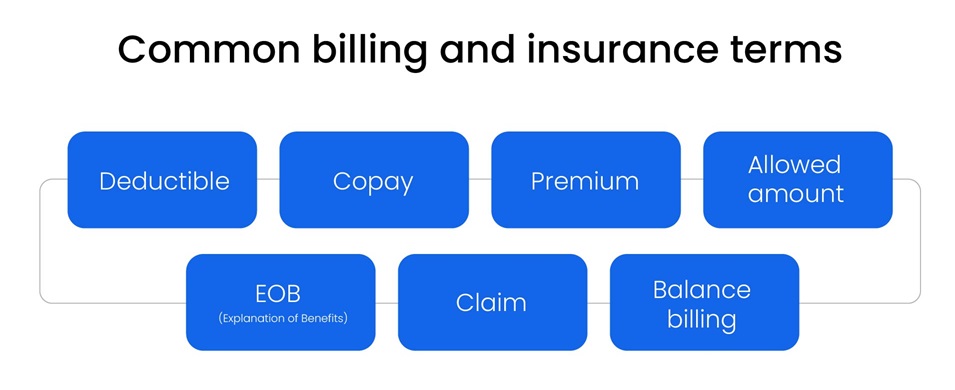
Deductible
The out-of-pocket amount a patient pays before their insurance begins to cover any medical expenses.
Example: A patient with a $1,000 deductible must pay the first $1,000 of their medical bills before insurance kicks in.
Copay
A fixed amount a patient pays for a healthcare service, typically at the time of service.
Example: A patient might pay a $20 copay for a doctor's visit while the insurance covers the rest.
EOB (Explanation of Benefits)
A statement sent by a payer to a patient explaining what treatments and services were paid for on their behalf. It details the amount billed by the provider, the amount covered by insurance, and the amount the patient owes.
Premium
The amount paid, usually monthly, for health insurance coverage. This can be paid by the individual, their employer, or a combination of both.
Claim
A payment request is one that a healthcare provider submits to the payer for services rendered. It includes details of the patient's diagnosis and the services provided.
Allowed amount
The maximum amount an insurance company will pay for a covered service. If the provider charges more than this amount, the patient may have to pay the difference, depending on their plan.
Balance billing
Billing a patient for the difference between the provider's charge and the insurance company's allowed amount usually occurs when patients receive services from out-of-network providers.
What is medical coding?
Medical coding translates healthcare diagnoses, procedures, medical services, and equipment into universal medical alphanumeric codes. The central coding systems used in medical coding include ICD (International Classification of Diseases), HCPCS (Healthcare Common Procedure Coding System), CPT (Current Procedural Terminology), professional and facility codes, and charge capture codes.
ICD codes
This coding system, currently in its 10th edition (ICD-10) and including 70,000+ unique identifiers, is used to classify and code all procedures, symptoms, and diagnoses recorded in conjunction with inpatient care in the United States. It is maintained by the World Health Organization (WHO). ICD-10 includes ICD-10-CM (clinical modification), which classifies diagnoses, and ICD-10-PCB (procedure coding system), which is for inpatient services.
CPT codes
CPT codes, maintained by the AMA (American Medical Association), describe medical, surgical, and diagnostic services. They are essential for billing outpatient and office procedures. CPT codes are accompanied by modifiers that specifically describe the services.
HCPCS codes
This system includes codes for procedures, equipment, and supplies not covered by CPT codes. It covers non-physician services like prescription drug use, ambulance rides, and durable medical equipment. It has two levels: Level I (CPT codes) and Level II (national codes used to identify supplies, services, and products not included in CPT).
Tip: You can also use modifiers with HCPCS codes to specify services further
Charge capture codes
Codes connect patient care services, physician order entries, and clinical items with chargemaster codes.
Note: Chargemasters are standard prices for items and services offered by healthcare providers. It is vital for healthcare providers to display their chargemaster sheet on their websites along with the prices of 300 services.
Charge capture codes include:
- Time reference codes.
- Billable items and supplies.
- Procedure descriptions.
- Departments involved in the medical services.
Healthcare providers use Chargemaster to negotiate reimbursements with the payers.
Professional and facility codes
It involves the translation of medical records into facility and professional codes.
Professional codes involve physicians and other clinical services delivered. These codes come from the patient’s medical record.
Hospitals use facility codes to record and account for the overheads and cost of healthcare services. This includes the charges for supplies, nursing staff, medical equipment, medication, and other technical care components.
Note: Professional codes are used by hospitals when a provider they employ performs a clinical service.
Integrating facility and professional codes eases the process for hospitals. Hospitals can leverage autonomous coding technology to improve their coding efficiency and stay compliant with HIPAA.
Why is accuracy important in medical billing and coding?
The revenue cycle management process begins with medical coding and billing. Accurate billing and coding ensure that the services offered are correctly documented and billed. Each medical code corresponds to a specific diagnosis or procedure, determining the reimbursement the healthcare provider will receive from insurance companies. Accurate medical coding and billing is vital for several reasons:
Correct payment
Payers rely on the codes submitted to determine the amount they will reimburse. Incorrect codes can lead to underpayment, overpayment, or claim denials.
Compliance
Maintains compliance with healthcare regulations and standards like HIPAA, avoiding potential legal issues.
Efficiency
Streamlines the billing process, reducing delays and the need for claim resubmissions or appeals.
Patient satisfaction
When claims are processed correctly and efficiently, patients receive accurate bills, enhancing their overall experience and trust in the healthcare provider.
Private insurance vs. Public insurance
Private insurance
Health insurance is provided through employer-sponsored plans or individual purchases from insurance companies.
Examples include plans from Blue Cross Blue Shield, UnitedHealthcare, and Aetna.
Public insurance
Government-funded insurance programs. The two primary public insurance programs in the United States are:
Medicare provides health coverage for people 65 and older and some younger individuals with disabilities. It has parts A, B, C, and D covering hospital services, medical services, Medicare Advantage plans, and prescription drugs, respectively.
Medicaid is a joint state and federal program that aids with medical costs for families & individuals with limited income and resources. Each state has its own guidelines and coverage options.
In-network providers vs. Out-of-network providers
In-network provider
Healthcare providers and facilities with a contract with a patient's health insurance plan to provide services at pre-negotiated rates. Patients typically pay less out-of-pocket when using in-network providers.
Out-of-network provider
Facilities and healthcare providers that do not have a contract with the patient's health insurance company. Using out-of-network providers usually results in higher out-of-pocket costs for the patient, as these providers may charge more than the insurance company's allowed amount.
What are the Types of Compliance and Regulations in Medical Billing and Coding?
HIPAA compliance
The Health Insurance Portability and Accountability Act (HIPAA) is a federal law that protects the privacy and security of patients' medical information. HIPAA mandates that healthcare providers, insurance companies, and business associates take specific measures to safeguard patients' protected health information (PHI).
HIPAA ensures that PHI is not disclosed to unauthorized individuals or entities. This includes physical safeguards like locked file cabinets and electronic measures like encrypted communications. HIPAA regulations protect PHI from being altered or destroyed in an unauthorized manner. Healthcare providers must implement measures to maintain accurate and reliable information. HIPAA also ensures that PHI is accessible to authorized individuals when needed. This includes having secure backup systems and disaster recovery plans.
The Affordable Care Act (ACA)
The Affordable Care Act (ACA) brought considerable changes to the healthcare system in the United States, including several impacts on medical billing and coding. The ACA offers health insurance coverage to millions of uninsured Americans, increasing the volume of claims submitted for reimbursement. The ACA emphasized adopting standardized coding systems, such as ICD-10, to improve the accuracy and efficiency of medical billing.
The ACA introduced value-based care models, focusing on the quality of care provided rather than the quantity. This shift required adjustments in medical billing and coding practices to ensure accurate reporting of quality measures and outcomes. The establishment of health insurance exchanges created new coding and billing requirements to handle the diverse range of insurance plans offered through these marketplaces.
Maintaining compliance with HIPAA, adapting to changes brought by the ACA, and preventing fraud and abuse are critical components of an effective medical billing and coding system. By following these regulations and implementing robust preventive measures, healthcare providers can ensure the integrity and efficiency of their billing practices.
How to ensure medical billing and coding accuracy?
Medical billing and coding are complex, and healthcare providers need to follow certain steps to ensure results. Here are tips for ensuring efficient medical billing and coding.
Stay current with medical coding and billing changes
The medical billing and coding field is dynamic, with frequent updates to coding standards and regulations. Staying current with regulatory changes is essential for several reasons. It ensures billing practices comply with the latest rules to avoid legal issues and penalties. Healthcare providers can maintain the accuracy of claims submitted to payers and ensure proper reimbursement. They can also streamline the billing process using the most current and efficient medical coding practices.
How do healthcare providers ensure billing and coding compliance?
Numerous resources are available to help medical billers and coders stay up-to-date with the latest changes.
- Organizations such as the AHIMA(American Health Information Management Association) and AAPC (American Academy of Professional Coders) offer training programs, certification courses, and regular updates on coding changes.
- Many institutions and online platforms provide continuing education courses specifically designed for medical billing and coding professionals.
- Subscribing to industry journals, newsletters, and websites can provide timely updates on coding changes, regulatory updates, and best practices.
- Attending workshops, webinars, and conferences can provide hands-on networking and training opportunities with other professionals in the field.
Leverage modern technology and software
Adopting technology in medical billing and coding can significantly enhance efficiency and accuracy.
EHR systems
EHR systems provide a comprehensive digital record of a patient's medical history, treatments, and outcomes. They reduce the risk of errors by maintaining detailed and accurate patient records. They enable easy access to patient information, improving coordination of care among healthcare providers. They streamline the documentation and billing process, reducing administrative burdens.
Practice management software
Practice management software (PMS) helps manage a healthcare provider's day-to-day operations, including appointment scheduling, billing, and claims processing. It automates routine tasks such as claim submission and follow-up, freeing up staff time for other responsibilities. PMS provides real-time updates on claim status, helping to identify and resolve issues quickly. Healthcare providers can use PMS tools to analyze billing data, identify trends, optimize revenue cycle management, and improve financial performance.
How do healthcare providers select the right automation tools?
Choosing the right technology for your practice involves careful consideration of your RCM needs and goals. Healthcare providers must start by evaluating their practice's specific requirements, including the volume of patients, the complexity of billing processes, and the level of integration needed with other systems. Next, they must compare different EHR and practice management software options, considering factors such as functionality, ease of use, and cost.
To keep the software current, healthcare providers must ensure that the vendor provides adequate training, support, and regular updates. They should choose a system that can grow with their practice and adapt to changing needs. Practices must seek feedback from other healthcare providers who have used the software to understand its strengths and weaknesses.
Ensure complete and accurate documentation
Thorough documentation is essential for effective medical billing and coding. Healthcare providers should ensure that all patient encounters are documented in detail, including symptoms, diagnoses, treatments, and procedures. Practices should document patient information as soon as possible after the encounter to ensure accuracy and completeness. They should utilize standardized templates and forms to ensure consistency and completeness in documentation. Conducting regular RCM audits to identify and correct any documentation errors or omissions also helps.
Maintaining detailed and accurate medical records is crucial for several reasons. They provide a complete picture of a patient's medical history, enabling providers to make informed decisions and deliver high-quality care. Accurate documentation can serve as a legal record in case of disputes or malpractice claims. Detailed records support precise coding and billing, ensuring proper reimbursement for services. Thorough documents facilitate continuity of care, especially when patients see multiple providers or transition between different care settings.
How do healthcare providers handle patient billing issues?
Effective communication with patients about their bills is essential for resolving billing issues and maintaining patient satisfaction:
- Provide clear and detailed billing statements that outline the services provided, the amounts covered by insurance, and the patient's responsibility.
- Inform patients about their financial responsibilities before services are rendered, including co-pays, deductibles, and potential out-of-pocket costs.
- Offer multiple channels for patients to contact you with billing questions, including phone, email, and in-person support.
- Provide options for payment plans to help patients manage their medical expenses.
How can healthcare providers resolve medical billing disputes?
Resolving medical billing disputes promptly and effectively is crucial for maintaining good patient relationships. Healthcare providers must take the time to listen to the patient's concerns and understand the root cause of the dispute. Clearly explain the charges, insurance payments, and the patient's responsibility. They should use straightforward language to avoid confusion. If an error is identified, promptly correct it and update the patient's bill. If a dispute is complex, it should be resolved at the initial level. Practices must also have a process to escalate the issue to a senior authority within the billing department.
How can healthcare providers manage coding errors?
Medical coding mistakes can lead to delayed payments, claim denials, and compliance issues. Identifying and correcting these errors is essential:
- Provide ongoing training for inpatient and outpatient coding staff to update them on the latest coding standards and practices.
- Implement autonomous coding software and tools that help identify potential errors and ensure accurate coding.
- Conduct peer reviews of coding practices to catch and correct errors before claims are submitted.
- Maintain a log of common coding errors and use this information to guide training and process improvements.
PCH Health offers comprehensive medical coding and billing solutions to help providers streamline their billing processes and improve accuracy. Our team of AAPC/AHIMA-certified specialty coders ensures accurate and compliant coding for all medical services, reducing claim denials and improving cash flow. We handle the entire billing cycle, from claim submission to payment posting, ensuring timely and accurate payments. By partnering with PCH Health, you can optimize your billing processes, ensure compliance, and increase cash flow. Contact us today to learn more about our revenue cycle management solutions and how it can benefit your practice.
